In our modern world, where medical science has made incredible strides, one of the most significant achievements in public health has been the development of vaccines. These remarkable substances have played a pivotal role in preventing the spread of infectious diseases and saving countless lives.
Understanding Vaccines
What Is a Vaccine?
At its core, a vaccine is a biological preparation that stimulates the immune system to recognize and fight off harmful pathogens, such as viruses and bacteria. Vaccines train the immune system to mount a defensive response by mimicking the actual pathogen’s presence. Training the immune system this way allows the body to remember the invader and respond quickly if exposed again.
How Do Vaccines Work?
Vaccines harness the power of the immune system’s memory. According to the World Health Organization, a vaccine typically contains a weakened or inactivated form of the targeted pathogen or its antigens. These molecules trigger an immune response. This introduction prompts the immune system to produce antibodies and activate immune cells. If the actual pathogen attacks in the future, the immune system recognizes it and launches a rapid and robust defense, effectively preventing disease.
With this foundation of what a vaccine is and how it operates, let’s delve into its primary objectives.
How Long Does it Take for Vaccines to Work?
After getting a vaccine, the immune system needs time to build protection against the disease. Generally, it takes a few weeks after vaccination for the immune system to develop a full and robust defense. Some vaccines require multiple doses to ensure long-lasting protection. For this reason, following the recommended vaccination schedule is essential to maximize effectiveness.
The Purpose of Vaccines
Vaccines provide a vital, multifaceted approach to preventing many of the world’s most devastating diseases. Their outsized impact stems from hundreds of years of research that has only accelerated with the modern understanding of the immune system’s complexities.
The principle behind vaccination is ‘preparation without the risk.’ Vaccines allow the immune system to learn, adapt, and arm itself without causing disease by introducing harmless fragments or weakened forms of pathogens. The process prepares the body for any potential encounters with the pathogen.
What Do Vaccines Aim to Achieve?
The primary goal of vaccines is to create immunity without causing illness, an important distinction detailed by the Centers for Disease Control and Prevention. Vaccinations protect both the individual receiving the vaccine and the broader community. They are vital for herd immunity, where enough of the population becomes immune to prevent the rapid spread of disease. Through herd immunity, even individuals unable to receive vaccinations for medical reasons benefit from this protective shield.
The Immune Response to Vaccines
Upon vaccination, the immune system goes into action. It identifies the vaccine’s foreign antigens and produces specific antibodies to neutralize them. Specialized immune cells work together to destroy the antigens and remember their structure, ensuring a swifter and more potent response in future encounters with the actual pathogen. Many scientific reviews, such as Fundamentals of Vaccine Immunology by Dr. Clem, detail the intricacies of the immune response to vaccines.
We outline the major players here:
- Antigen-presenting cells (APCs): These cells capture the antigens present in the vaccine – often fragments of the pathogen’s surface proteins. Then they display them using major histocompatibility complex (MHC) proteins on their surfaces. This display acts as a “wanted poster,” allowing other immune cells to bind the antigen and identify the intruder.
- B cells: B-lymphocytes, a type of white blood cell, recognize the displayed antigens and initiate the production of antibodies. Antibodies are Y-shaped proteins that lock onto specific antigens like puzzle pieces. This antibody-antigen binding neutralizes the pathogen and marks it for destruction by other immune cells.
- T cells: T-lymphocytes, another key immune cell type, contribute to vaccine-induced defense in multiple ways. Helper T cells (CD4+) assist B cells in inducing an immune response and activating other immune cells. Cytotoxic T cells (CD8+), on the other hand, directly target and eliminate infected cells.
- Memory cells: One of the most astounding aspects of the immune response to vaccines is establishing immunological memory. As B and T cells respond to the vaccine, some differentiate into long-lived memory cells. These memory cells “remember” the pathogen’s unique features, ensuring a rapid and potent response if the actual pathogen is encountered in the future.
The immune response doesn’t end with the initial encounter. The immune system continuously refines its tactics. It generates diverse antibodies and immune cells to combat potential threats. Over time, the immune response may wane, but memory cells remain vigilant, capable of reactivation if needed. This is why booster shots are sometimes required to reinforce immunity and maintain protection.
Now that we have explored the immune response to vaccines, let’s examine the various types and compositions of the vaccine arsenal.
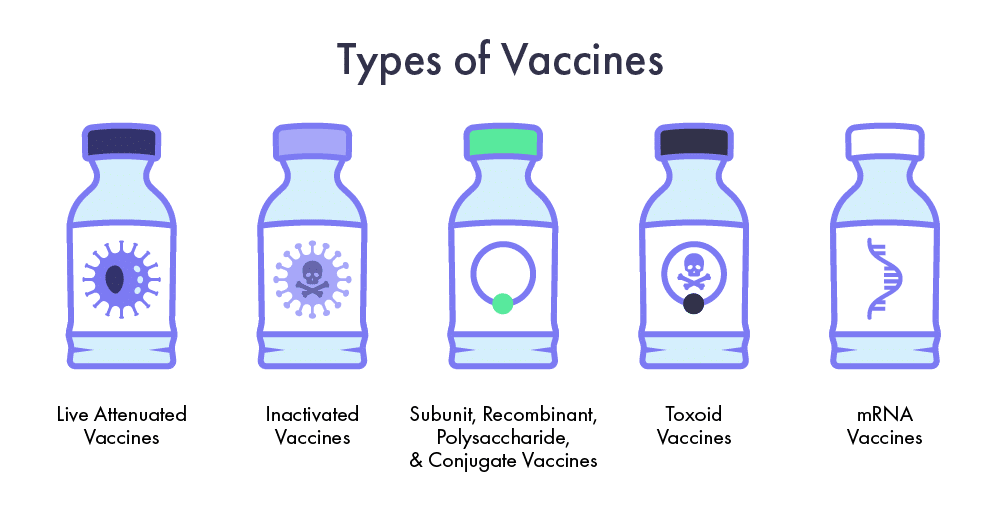
The Vaccine Arsenal: Types and Composition
Vaccines come in many forms, each carefully designed to elicit a specific immune response tailored to the pathogen. Each type uses a unique strategy to help the immune system recognize and fight potential threats.
Live Attenuated Vaccines
Live attenuated vaccines contain a weakened version of the actual pathogen that is still capable of replicating but is much less virulent. These vaccines imitate a real infection, helping the immune system give a strong response. Immune cells meet the live pathogen, produce antibodies, and create immune memory.
Examples of live attenuated vaccines include:
- Measles, Mumps, and Rubella (MMR) Vaccine: This vaccine contains weakened forms of the viruses that cause these diseases. It has been instrumental in reducing the prevalence of these once-common childhood illnesses.
- Varicella (Chickenpox) Vaccine: By introducing a weakened varicella-zoster virus, this vaccine provides immunity against chickenpox and, importantly, the risk of shingles later in life.
Inactivated Vaccines
Inactivated vaccines contain pathogens that have been killed or altered, rendering them non-functional. While these vaccines may not produce as robust an immune response as live attenuated vaccines, they are safer for individuals with compromised immune systems or certain health conditions. Examples of inactivated vaccines include:
- Polio Vaccine: The inactivated poliovirus vaccine (IPV) has been pivotal in the global efforts to eradicate polio. It effectively trains the immune system to recognize and fight the poliovirus without causing the disease.
- Hepatitis A Vaccine: By using inactivated hepatitis A virus, this vaccine protects against the highly contagious liver disease. While most cases of Hepatitis A resolve on their own, some lead to severe consequences, permanently altering liver function.
Subunit, Recombinant, Polysaccharide, and Conjugate Vaccines
These vaccines focus on specific pathogen components, such as proteins or carbohydrate chains, to trigger an immune response.
- Hepatitis B Vaccine: This vaccine contains a single antigen—a recombinant protein from the hepatitis B virus—to stimulate immunity. It is a prime example of a subunit vaccine and has been instrumental in reducing hepatitis B infections worldwide.
- Pneumococcal Conjugate Vaccine: This vaccine combines a piece of the bacterial coating (polysaccharide) with a carrier protein to address bacterial infections like pneumonia. This conjugation enhances the immune response, especially in infants and young children.
Toxoid Vaccines
Toxoid vaccines provide immunity to diseases caused by toxin-producing bacteria using inactivated toxins to stimulate an immune response. An example is the Diphtheria-Tetanus-Pertussis (DTaP) Vaccine, which safeguards against diphtheria and tetanus by utilizing inactivated toxins.
mRNA Vaccines
Based on a decade of research, mRNA vaccines are a groundbreaking innovation that became prominent during the COVID-19 pandemic. They use a small piece of genetic material from the pathogen to instruct the body’s cells to produce harmless antigens that mimic those produced by the virus, triggering a robust immune response.
- COVID-19 mRNA Vaccines: The COVID-19 vaccine employs lipid nanoparticles to deliver a snippet of the virus’s genetic material in the form of mRNA. The mRNA instructs cells to produce the spike protein found on the SAR-CoV-2 virus’s surface, teaching the immune system to recognize and neutralize the virus.
- Influenza mRNA Vaccines: Recent studies by vaccinologists, like Arevalo et al.’s pivotal work in mice and ferrets, demonstrate the expanded potential of mRNA technology to prevent other diseases. While these vaccines are still developing, they may soon revolutionize seasonal flu protection by swiftly adapting to new strains, offering a more flexible approach to vaccine development.
Building Blocks of Vaccines
Beyond the specific pathogen components, vaccines often contain additional elements to optimize their effectiveness and safety:
- Adjuvants: These substances are added to vaccines to enhance the immune response. They stimulate immune cells at the injection site, leading to a stronger, longer-lasting defense. Aluminum salts are a typical example of adjuvants.
- Stabilizers and Preservatives: Stabilizers are added to vaccines to ensure they remain effective during storage and transportation. Preservatives prevent microbial growth in multi-dose vials, extending the vaccine’s shelf life.
- Trace Amounts of Antibiotics: Some vaccines include antibiotics in their formulation to prevent bacterial contamination during manufacturing and injection.
As we unravel the immune system’s complexities and grow our understanding, we’re also exploring innovative delivery methods. Vaccine technology will evolve, promising even more precise and effective ways to protect against infectious diseases. The vaccine arsenal is a testament to humanity’s commitment to securing a healthier future through historical knowledge, cutting-edge science, and ongoing research.
Traditional Vaccine Limitations
While traditional vaccines have undoubtedly transformed public health and prevented numerous diseases, they have their own limitations. These challenges have spurred scientific inquiry and innovation, developing novel approaches to overcome these hurdles.
Pathogen Mutations and Waning Immunity
One notable limitation of traditional vaccines is their vulnerability to pathogen mutations. Some viruses, such as the influenza virus, mutate rapidly. As a result, they produce new strains. These new strains may evade the immunity induced by existing vaccines. Such changes in the virus mean that flu vaccines need to be reformulated every year to match the prevalent circulating strains.
Additionally, the protective immunity elicited by certain vaccines can wane over time. For instance, immunity from pertussis (whooping cough) vaccines may decrease after several years, leaving individuals susceptible to infection again. These challenges highlight the importance of vaccines that offer more enduring protection.
Adjuvant-Associated Side Effects
Traditional vaccines frequently use adjuvants to boost their effectiveness. While they promote a robust reaction, adjuvants might cause side effects like localized pain, swelling, or fever at the injection area. Research continues to find adjuvants that reduce these effects but keep the vaccine effective.
Cold Chain Requirements
Traditional vaccines need stable conditions during storage and transport. Many vaccines are sensitive to temperature fluctuations and require a consistent cold chain to remain potent. In places where it’s hard to find reliable refrigeration, this sensitivity makes things challenging, affecting whether people can get the vaccine and its effectiveness.
Revolutionizing Vaccine Delivery With Nanoparticle-Based Products
Nanoparticle-Based Delivery: A Breakthrough Solution
Scientists are working on new ways to make vaccines more effective and stable. One groundbreaking approach uses peptide nanoparticle-based drug delivery products, exemplified by companies like Phoreus Biotech and their Amphipathic Peptide Capsule (APC) technology.
Enhanced Stability
Peptide nanoparticles in these delivery systems have many benefits. They protect vaccine components from breaking down, making them more stable. This is especially helpful for vaccines sensitive to environmental factors like heat, water, or oxygen.
Targeted Delivery and Immune Activation
Scientists design nanoparticle-based systems to target specific immune cells. By combining vaccine antigens with these nanoparticles, researchers can direct the immune response more effectively, potentially leading to a stronger and more focused defense against pathogens.
Reduced Adjuvant Dependence
An exciting prospect of nanoparticle-based delivery is its potential to reduce the reliance on traditional adjuvants. Certain nanoparticles have unique properties that stimulate the immune system, possibly reducing the need for additional adjuvant compounds. Phoreus peptide nanoparticles on the other hand do not stimulate the innate immune system thus leaving open the option to select the optimal adjuvant for each specific disease. These advancements will ultimately lead to vaccines with fewer side effects and strong protective efficacy.
Broad Applications
Nanoparticle-based delivery goes beyond just infectious disease vaccines. Researchers are exploring nanocarrier use in cancer immunotherapy, personalized medicine, and the delivery of genetic material for gene therapy. At Phoreus Biotech, challenges with traditional vaccines have ignited our drive for fresh solutions. We’ve pioneered novel methods such as peptide nanoparticle-based drug delivery and associated cell transfection products. These advancements address the challenges of pathogen mutations, adjuvant-related side effects, and cold chain requirements.
As science continues to evolve and our understanding of immunology deepens, these innovative strategies offer a glimpse into a future where vaccines are even more effective, accessible, and tailored to the diverse needs of global health. While we honor the achievements of traditional vaccines, we eagerly anticipate the next chapters in medical science, fueled by a steadfast dedication to protecting global health and wellness.
Jump into the pipeline of medical advancements with Phoreus’ targeted amphipathic peptide capsule nanocarrier technology. Contact us today to discover how we can help you deliver molecular payloads with stable, non-immunogenic, and easily metabolized precision.